Christians might seriously consider Ellen White’s urging to understand and follow the principles of health.
Warren A. Shipton
Part 2
The angel messengers brought to view by the apostle John in Revelation 14 provide two significant emphases. Acknowledging God’s activities and then worshiping the Creator-Savior is the first response urged. The second follows naturally in that these revelations are to be shared with unwarned members of the human family (vss. 6, 7). Readers are also urged to contrast life as originally planned by God following creation with the practices in the unregenerate world (Babylon) and respond to the invitation to make significant lifestyle changes (vss. 8–12). Christ similarly indicated to His disciples that self-indulgence and frivolity would prevail in society near the end of time, just as before the judgment of the universal flood (Matt. 24:37, 39).
Ellen G. White’s health vision outline (recorded 1864/1865) was set in the context of Eden, the Fall, and the contributions of humans to disease and suffering observed as a result of ignorance or disregard for the principles of health. She later indicated that it was the duty of Christians to understand these principles so that mind and body are in the best condition to enable believers to bring glory to God. This is essentially an acknowledgment that Christ designed and then purchased our bodies as His property, hence frustrating the claims of Satan to ownership. Once understood, the principles of health are ours to follow as precious light.
Christians and others have understood something of the principles of health from early times. Daniel and his friends were early exponents of vegetarianism (Dan. 1:8, 16). More recently, in the United States there were prominent health movements from 1800 to 1870. Many of the themes introduced in Ellen G. White’s health vision had been and were expressed by these movements. The key to the lasting nature of the Adventist emphasis, which gained momentum only after the 1863 vision, was achieved by linking health to spiritual values. Understanding and rendering obedience to the laws of health was regarded as a sacred responsibility. The concept that the principles of health were to be studied and reform effected to enable clear thinking was emphasized by Mrs. White in 1873. Health reform practiced among believers would enable them to grasp great Bible truths, work to fit them for heaven, and enable them to be good ambassadors of the gospel to others. This work was inseparably connected with the proclamation of the three angels’ messages.
To a variable degree, Adventist communities have practiced the principles established through God’s prophetic agencies. An early American Cancer Society study (1959) showed that the death rate among Adventists of that time was well below that of the general population in California. Death from heart disease, stroke, cancer, and diabetes was in the range of 45 to 55 percent of other community members. International studies conducted in Japan, Netherlands, and Norway confirmed these trends. Life expectancy was improved by exercise and when weight control was given priority. Believers also accepting an essentially vegetarian lifestyle had a life expectancy in the region of a decade longer than those preferring little exercise and consuming red meat, fatty foods, eggs, and coffee.1 The principal reasons for increased life expectancy appeared to be the intake of fruits, vegetables, and nuts with their phytochemicals, unsaturated fats, and abundant dietary fiber content. An interesting comment made during a major study on the association between diet and heart disease and cancer was that when poor health began to be experienced, individuals in the Adventist tradition tended to move toward the dietary habits recommended for vegetarians.2
When different types of vegetarianism were investigated within Adventism in relation to the incidence of Type 2 diabetes, vegans were the least likely to contract the disease followed by lacto-ovo vegetarians and other types of vegetarians (pesco- and semi-vegetarians). The first two types of vegetarian lifestyles were protective against the disease.3 Moving outside Adventist circles, the consistent results shown by practitioners of a vegetarian lifestyle were lower incidences of hypertension, coronary heart disease, and mortality. Type 2 diabetes was less frequent, too, as body weight control was more achievable.4
In many countries, infectious diseases no longer pose the enormous challenges that they did in previous centuries. However, there is now a rise of lifestyle diseases, which is coincidental with urbanization, globalization, and the adoption of poor Western dietary choices. Uncontrolled appetite and the lack of exercise are the scourges of modern societies.
The sobering reality is that in 2017, an estimated 70 percent of the global incidence of disease was attributed to non-communicable diseases.5 The most significant are cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes. The risk factors are an unhealthy diet, tobacco use, alcohol abuse, and physical inactivity.6 Poor health caused by overnutrition and obesity through eating animal products and increased consumption of refined foods and fats contrasts with the continuing problem of undernutrition in some locations or among disadvantaged groups.7
Just as Moses enunciated principles of health for the Israelites during the Exodus, enabling them to be fit representatives of God’s truth, so today additional information has been given fitting believers to be good ambassadors for Christ. This is a necessary prerequisite to enable them to handle the “momentous truths” relevant to the end times (see also 1 Peter 2:9).8 As a consequence, our understanding and practice of the principles of health should be well in advance of others who do not accept the Bible as their guide, which reveals God’s purpose to restore His image in the human race.
The invitation is for the experience of good health to be more widely shown among believers and others willing to embrace the vision and experience the blessings promised by God. The challenge given to those with talents spoken of by Jesus (Matt. 25:14–39) comes again to us today. If the usefulness of our talents is blunted or the period of their functionality shortened by practices contrary to the principles of health, then loss will be suffered.
Principles of Life/Health
Ellen G. White spoke often about the laws governing health. At times, she referred to these as rules and principles.9 By this she meant that informed decisions about maintenance of health could be made by reasoning from cause to effect. From such observations, one is then able to formulate operational principles so as to give optimum health. She identified several of these principles.10
Today we tend to avoid the use of the term laws because scientists and philosophers often contend that the explanations offered in biology do not indicate causality but rather relate to function. Nevertheless, there are a few well-understood laws in genetics. On account of these understandings, terminology adopted in this article will speak of “operational principles” rather than “laws.”
Ellen White took the Exodus experience as her reference point in the health vision and God’s instruction given there for developing an understanding of their significance. These principles are designed to assist in enjoying a pleasant life and a vigorous spiritual experience. The operational principles during the Exodus event identified here in the area of physical health are shown in Table 1.
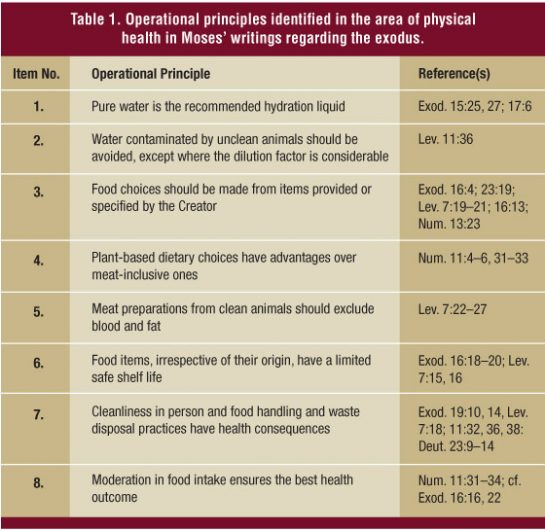
This table in no way suggests that physical health is not affected by the mental state, the social surroundings, or the spiritual state. The vision of 1863 (1865 statements) affirmed the above principles with the exception of Items 2 and 6. The last principle was supported later (1887) by Ellen White.11 Her tacit acceptance of Principle 2 might be assumed as she traveled. The reasoning is that wherever municipal water supplies are used for domestic purposes, it is inevitable that contamination occurs, for the catchment area will always contain adulteration from many contaminating sources. Nevertheless, at the same time as this dynamic was playing out, she spoke frequently of the use of pure water in such places; one can assume that tank water or clean well water was not always available.
She also expanded readers’ understanding of some of these principles and gave other helpful ones as the years passed.
Diet Chosen May Predispose to Disease
Warning against the use of animal-based foods arguably carries with it the message that dietary items may predispose to disease or carry disease agents. Without specific statements, however, it is difficult to attribute emphasis. It seems that Ellen G. White’s frequent emphasis was on meat carrying disease-causing agents, but occasionally she used language that indicated that predisposition occurred through food choices. Several examples of the latter are as follows: “Indulgence in eating is too frequent. . . . The blood becomes impure, and then diseases of various kinds occur”12 (1864).
If parents and children eat frequently, irregularly, and in too great quantities, even of the most healthful food, it will injure the constitution; but in addition to this, if the food is of an improper quality, and prepared with grease and indigestible spices, the result will be far more injurious13 (1865).
The liability to disease is increased by flesh eating14 (1890).
“They [those who have adopted health reform] will realize that the use of food which they formerly regarded as harmless, was slowly but surely laying the foundation for dyspepsia and other diseases”15 (1909).
Two questions need to be asked. Did her statements represent ideas in advance of their times, and are they correct? First, it must be acknowledged that the idea of dietary habits contributing to cancer and other disease development was a rather natural outcome of the “humor theory” of disease. In an attempt to get the humors back into balance, diet was one of the mechanisms recommended.16 Added to this, forms of quackery involving dietary supplementation were practiced in Ellen White’s time. One of the prominent and more reasonable health exponents of the early 19th century, Sylvester Graham (1794–1851), was explicit about moderation, vegetarianism, and the use of natural food items rather than refined foods. He opposed the use of condiments and pastries, too. He contended that vegetarianism was well suited to meet human needs because the Creator had arranged the body for that purpose.17 This means that no particular priority claim can be attributed to Ellen White and, of course, there are insufficient details to allow analysis of all the factors involved.
Today, it is rather well recognized that dietary availability and choice predispose to disease. The influence of diet on the incidence of disease was highlighted before the end of the 19th century, although writers did not nominate the level of contribution made by dietary predisposition compared to other factors. Though some of the studies likely would not pass modern scientific scrutiny, it is the suggestion that is of interest here. It remained for latter generations of scientists to show the relationship among host, pathogen, and environmental influences. Not only the components involved in food intake, but also the quantity have a bearing on disease incidence.
Heart Disease
Today there is greater understanding about heart disease, including the fact that the risk is increased through excessive fat intake, use of animal fats, and high sodium intake. On the other hand, the risk is diminished by whole grains, nuts, fruit, vegetables, and fish. All this is not without controversy, as may be imagined.
Diet and Disease Risk Discovered. The association of lesions in the arteries and cholesterol was understood in the West by 1946, but most considered this a normal part of aging. This concept was so rigidly held that clear experiments completed in Russia in 1913 establishing a link were ignored. The role of diet in reducing the risk of coronary heart disease came in the 1960s, although again, there was evidence of its effectiveness as early as 1916–1922. These and other studies to follow were not well known, not fully appreciated, or rejected vigorously. Even in the 1960s, controversy dogged the idea that attention should be given to lowering the cholesterol level through dietary avenues in order to reduce cardiovascular disease.18
The early clues to the influence of diet on disease came from comparisons of disease incidences in those on simple diets that were essentially vegetarian. The historical records contain a rather extensive account of suggestions that diet and disease were connected, but the evidence featuring in its support was often rather tenuous. Against this background, the following statement was penned by Ellen G. White in 1896, which indicates she gave Moses’ writings priority and God the credit:
“The meat is served reeking with fat, because it suits the perverted taste. Both the blood and the fat of animals are consumed as a luxury. But the Lord gave special directions that these should not be eaten. Why? Because their use would make a diseased current of blood in the human system. The disregard for the Lord’s special directions has brought a variety of difficulties and diseases upon human beings. . . . If they introduce into their systems that which cannot make good flesh and blood, they must endure the results of their disregard of God’s word.”19
A large intake of fatty foods is not a good choice. This was understood by one people group anciently (Jewish), where the advice was given to avoid eating animal fat (Lev. 7:23). At a rather later time (600 B.C.), the Indian physician Charaka specifically noted the link between heart disease, overeating, lack of exercise, and stress.20
Heart Disease Today. The relationship between heart disease and fat intake is not free from dispute in scientific circles. A number of studies have shown that the risk of heart disease is reduced by limiting the intake of fatty foods containing saturated fats and replacing them with unsaturated fats and at the same time taking on a diet high in fiber and micronutrients from fruit and vegetables. And it is not only heart disease that is affected by fat intake―obesity and colorectal cancer risks may also be increased.21 In terms of general health, Ellen G. White gave advice along these lines, too. She advised using an abundance of fresh fruit and vegetables and abstaining from fat-laden items of food.22
Particular classes of saturated fatty acids have different effects, so sweeping statements can no longer be made about saturated versus unsaturated fats. The jury is still out on the intake of coconut and palm products, which are exceptional in the plant kingdom in that they contain a high proportion of saturated fats. The following information should help readers to form an opinion:
The richest source of saturated fats is the oil from these plants. The composition of palm oil differs considerably from coconut oil. The latter oil has a high percentage of fatty acids that increase good cholesterol (high density lipoproteins), although some of its fatty acids raise low-density lipoprotein levels. The overall effect in populations eating significant amounts of coconut products differs depending on the other components of their diet. For example, the Kitavans (Melanesia) have a low incidence of coronary heart disease, whereas groups from Sri Lanka have a relatively high incidence. The difference between the populations is thought to be attributable to the high intake of fish, fruit, and vegetables, and the traditional absence of processed foods among the Melanesians. Complex interactions occur among nutrient components, and sociological factors also come into play. This means that combining a Western diet with the intake of all but small quantities of coconut products could be problematic, especially if coconut oil is chosen as a significant food item. Coconut oil is to be preferred over butter, but it does not compare favorably with vegetable oils.23
The risks of consuming palm oil with its high levels of saturated fatty acid have not been fully assessed, but it appears to be relatively risk-free as long as there is not an excess level of dietary cholesterol present in the diet.24 The oil when freshly prepared contains powerful antioxidants, which gives a clue to its relatively neutral impact on heart disease. However, when the oil is repeatedly reheated (a common practice in Asia) some of the beneficial properties are lost, allowing its use to increase the risk of heart disease, at least in animal models.25 When all the data are considered, there are perhaps better options than using palm oil, as demonstrated in animal experiments. Extra virgin olive oil actually decreased disease lesions when fed to mice (diet mimicked Western), whereas palm oil-fed animals showed accelerated lesion formation.26
If we are in a position to lower our cholesterol levels, this will be beneficial in reducing the risk of vascular and heart disease. The heart damage risk marker cholesterol (some is needed by the body) can be lowered by reducing the intake of eggs, meat, and full-fat dairy products (including cheese). Fish is exceptional in that it contains beneficial Omega-3 polyunsaturated fatty acids (good plant sources are found in nuts and beans); but on the other hand, it still contains a reasonable quantity of cholesterol.27 When considering the level of one risk factor in the diet, careful readers will be aware that substitutes should contribute toward healthful eating. For example, reduction in saturated fats should not be associated with a compensatory increase in refined carbohydrates.28
As to meat in the diet, it recently has been suggested that the tendency for red meat to increase the risk of heart disease may be the result of additional substances found in abundance in this food item. The first of these is carnitine. It is in relatively high concentrations in red meat, especially lamb (also in dairy products). This substance is changed by microbes in the body. Such changes tend to become an issue in those individuals with a low fiber intake, for metabolites are produced that increase the risk of certain heart diseases. The body normally produces all the carnitine it needs to carry out its functions of transporting fatty acids, so there is no need to worry about including it in the diet.29 Then there are the advanced glycation end products formed through reactions between protein and sugar groups during metabolism in the body or in highly heated, processed foods (browning during baking, grilling, barbecuing, etc.). The components are abundance in foods rich in protein and fats, especially those of animal origin. Their presence has been associated with diseases such as atherosclerosis and chronic kidney disease. These findings constitute additional incentive to reduce one’s dependence on animal-based foods.30
Other dietary components contribute to heart health. Olive oil is an important component of the Mediterranean diet. Ellen G. White gave this food item a good report sheet.31 This monounsaturated fatty acid (major component is oleic acid) exerts a number of health benefits, and some of these are due to the presence of antioxidant agents (polyphenols). Olive oil decreases the levels of low-density lipoproteins and total cholesterol. High-density lipoproteins (good ones) and cholesterol levels remain unchanged.32 Many benefits have been attributed to including this oil (particularly high-quality lines) in the diet. These include decreasing the risk of atherosclerosis and the risk of contracting certain cancers. Additional benefits have been claimed for those who have diabetes, rheumatoid arthritis, gastric ulcers, and gall-bladder problems.33
The good news is that the effects of poor choices can be lessened through exercise, stress management, and dietary decisions that reduce fats. The use of polyunsaturated fats (e.g., corn, safflower, and soy) or monounsaturated oils (e.g., canola, olive, and peanut) may be of benefit, too. Foods rich in Vitamin E (seeds, nuts, and vegetable oils), carotenoids (organic pigments), and flavonoids (compounds that exert changes in the female reproductive organs during the oestrous cycle and promote development of female secondary sexual characteristics), reduce the formation of dangerous types of low-density lipoproteins. Flavonoids are present in fresh, ripe plant foods and berries, particularly in the peels. The yellow, orange, and red pigments associated with fruit and vegetables are carotenoid pigments. Eating plenty of fresh fruit and vegetables and regularly consuming nuts will help to lower the risk of heart disease. The soybean and its products are especially valuable in lowering blood cholesterol levels.34
Maintaining cardiovascular health is not only about diet. Exercise and other forms of physical activity are also significant. It has been estimated that about half of the population in industrialized countries place themselves at increased risk of premature death from heart and other diseases due to a lack of physical activity. Health benefits can be reaped from moderate levels of physical activity undertaken on a regular basis. The death rate drops with a walk of 1.6 kilometers (one mile) per day. Further benefit is not observed after 4.8 kilometers (three miles). Recommendations other than walking involve participating in moderate or vigorous activity three to five days per week.35
Type 2 Diabetes
Diabetes is of ancient origin, and attempts to treat it by imposing dietary regimes began more than two centuries ago. The variations in suggested solutions were wide, but one common element was the belief that restricting the quantity of food taken was the key to curing the disease. Exercise was also found as useful in its treatment. Ellen G. White never mentioned diabetes by name but may have treated it under the title of dyspepsia as some others did. Nevertheless, she often spoke against some of the root causes of Type 2 diabetes—gluttony, cakes, and other rich foods with their load of sugar.36
Diabetes Today. Diabetes increases the risk of heart disease, kidney dysfunction, blindness, nerve disease, and limb amputation. In Type 2 diabetes, blood glucose levels are elevated because the body cells do not respond normally to insulin. This hormone allows cells to use glucose to obtain their energy, but in this type of diabetes, glucose is not absorbed properly by the cells.37
Type 2 diabetes is of growing public health interest in many places, particularly Western nations, but the trend is seen in the Asia-Pacific region as well. There is a veritable epidemic in China and India. Type 2 (or non-insulin-dependent) diabetes can be prevented or delayed through managing the risk factors. Reducing the amount of body fat and being physically active are key strategies to adopt to prevent Type 2 diabetes and to treat diabetes successfully.
Evidence suggests that the intake of high levels of saturated fats during pregnancy compromises the future health of the baby. Avoiding excessive levels of saturated fats, highly refined foods, and realizing the value of grains and vegetables are important parts of any successful strategy.38 God’s initial plans for the human race included both participating in regular exercise and eating exclusively of fresh foods. Refined foods were not available (Gen. 1:29; 2:15; 3:18, 19), making it likely that diabetes was unknown to early humans. Ellen White’s advice was for the underactive to exercise in fresh air, for the excessively active to be more moderate, and to follow God’s initial dietary plan for the race.39
Blood glucose control is made simpler by eating starchy, high-fiber carbohydrates. Simple carbohydrates found in honey, soft drinks, sweets, biscuits, fruit drinks, and the like are best avoided or taken in small quantities. It is best not to overload on proteins and to keep fats under control. It is wise to eat less and not to eat in front of the television or computer. The advice is to reduce fatty and sugary foods and second helpings. In other words, there is a need to take control of one’s eating.
Vegetarians are at less risk of developing Type 2 diabetes in contrast to meat eaters. In fact, there is a positive relationship between how much red meat and processed meat that is eaten and diabetes. The suspect compounds are called advanced glycation end products (formed from interactions between sugars and amino groups on proteins and the like). These are found naturally in some foods, especially those high in protein and fats of animal origin. Cooking at high temperatures and dry heat ensures they are present in especially high amounts. There is also a gentle warning that caffeine intake in the form of coffee, tea, and cola drinks is a risk factor for Type 2 diabetes and could exacerbate it in those already showing symptoms of the disease.40
The key to understanding blood glucose levels resides in understanding the glycemic index. This index is a system of classifying carbohydrates in terms of how quickly and strongly they cause blood sugar to rise. The higher the index value, the more caution is needed in the use of the food item, for regular strong blood glucose spikes are bad for health. The glycemic index is raised by eating highly processed products. The more finely ground a product, the higher its value on the index. The good news is that foods can be chosen wisely by consulting the index on the Internet.41 The general advice for those without this facility is to use minimally processed foods and largely avoid sugar and soft drinks. It’s important to note that some fruits are rich in natural sugars but do not raise blood-sugar levels as strongly as some starchy foods. How the sugar is packaged in the food is thus important. Dietary fiber (soluble and insoluble forms) play important functions in human health. Soluble fiber particularly appears to convert carbohydrates into a slow release form that lowers the insulin required for uptake into tissues. This and other factors contribute to reducing the risk of diabetes and other diseases.42
It is important not to fall into a common trap of thinking that simple sugars such as fructose and glucose found in honey are less damaging than cane sugar (sucrose) or other simple sugars. All simple sugars are problematic when taken in excess. Scientists warn that there is a tendency to overweight and other problems through eating food and drink loaded with simple sugars.
Gastric Upset, Ulcers, and Cancer
One of the most common 19th-century conditions was dyspepsia (bad digestion). In its severest form, it was manifested as gastric or duodenal ulcers. Dyspepsia of the stomach, intestines, and liver were diagnosed. As early as 1866, one medico (Austin Flint) indicated that a proper diet, regularity in eating, and avoiding excesses, together with psychological support, would go a long way toward overcoming this condition.43 He may have been influenced in his writing by William Beaumont’s prior reports on his famous experiments performed on the gunshot victim Alexis St. Martin. Through a fistula into Alexis’ stomach, Beaumont was able to observe the effects of various food items on the activities of the stomach. He observed that particularly spicy condiments, tea, coffee, and alcohol debilitated it. He declared that dyspepsia was often caused by overeating and drinking.44
Similar advice appeared in Ellen G. White’s writings, though she may have used other sources for her statements. It is undeniable that parallel thoughts were circulating at the time she wrote, but on balance a lot of unusual and useless advice was being promoted, too.
Dyspepsia and Associated Conditions Today. Dyspepsia was one of the great scourges of the 19th century. Today, it is estimated that 30 to 40 percent of U.S. adults experience upper abdominal pain or discomfort. Such pain may be associated with acid reflux, peptic ulcers, malignancy, or other causes. Many experience acid reflux. This is where the gastric contents are released into the esophagus, leading to discomfort. The release is caused by impaired function of the special muscle at the lower end of the esophagus that is meant to prevent escape of gastric juices. Not surprisingly, this release of acid into unprotected tissues damages them. The experience is more common in the West than in other regions of the world. The lifestyle risk factors involved appear to be obesity, smoking, alcohol, fatty and fried foods, tomato sauce, mint, garlic, onion, coffee, and chocolate. Large meals eaten less than three hours before lying down are an invitation to experience reflux. Tight-fitting clothes should be exchanged for more loose-fitting gear to lessen the risk. If the condition is neglected, ulcers and esophageal cancer development can be anticipated in some individuals. One line of advice is to effect lifestyle changes, but most do not respond positively to this advice and require more extreme measures. One practical option adopted by the author with success was to eat the evening meal early and make it light. Avoiding acid foods, including those containing vinegar (acetic acid), also helped. This, on reflection, was essentially Ellen White’s advice as well as that of experts,45 and would have prevented considerable discomfort if I had taken notice earlier. Simpler acids, such as acetic acid, delay stomach emptying and in some individuals their intake appears to be connected with increased risk of acid reflux.46
Gastric Ulcers and Cancer. The question sometimes arises: Do fiery spices harm the body? Beaumont had shown at an early date that they debilitated the stomach. Ellen White indicated that spices irritate the stomach lining, which is not a particularly radical idea as experience shows that when these spices contact the mouth and other such delicate tissues then irritation/inflammation occurs. Many spices are irritants according to common experience, a feature recognized by Ellen White,47 and this is substantiated by detailed scientific evidence. Spices such as pepper, chili, and mustard irritate the stomach; or in other words. make it difficult for the cells to operate in a balanced manner. When irritation is through this means is combined with a stressful lifestyle, the way is opened to damaging the mucosal lining in the stomach. This makes the organ susceptible to ulcer formation. Scientific research suggests that eating highly seasoned food (e.g., high consumption of chili and other hot spices) on a regular basis is not a wise choice. Too many associations have been found between the incidence of different kinds of cancer and the intake of very spicy foods to make their consumption advisable, although it is important to note that not all studies support this line of thought.48
Another association of interest is the consumption of Chinese/Cantonese-style and similarly prepared salted fish. These fish are prepared by placing crude dry salt or concentrated brine in contact with the meat; the meat may be left to decompose slightly before salting occurs. In various geographical regions, where consumption of this product is traditional, unusual occurrence of cancer of the upper respiratory tract has been noted. This has been related to the volatile N-nitrosamine compounds identified in the product. Eating such food is associated with a high incidence of disease. Hence, Cantonese-salted fish are classified as a Group 1 carcinogen (highest level). The risk for stomach cancer is increased through eating such highly salted food.49
On a more general level, it has been found that increasing the amount of fruit and Vitamin C and decreasing the intake of salt and salted foods had a positive influence on the prevention of gastric cancer. Salt is known to enhance the effects of known gastric carcinogens, and destroys the protective barrier of mucus on the stomach wall, making the association very plausible.50 This, interestingly, was the advice given by Ellen G. White. Though she advised not to eat largely of salt, she recognized the need for some.51 This in no way is a claim of hidden knowledge or priority.
Cancer Latency Broken
There is another insidious side to cancer development. Referring to the indoor lifestyle and personal habits, particularly of females in her day, Ellen G. White wrote: “Cancerous humor, which would lay dormant in the system their life-time, is inflamed, and commences its eating, destructive work.”52
Virus Latency. The latency of viruses was recognized in the 1950s when experiments with mouse leukemia virus were carried out involving selected inbred strains of mice. The virus was shown to be transmitted to the offspring, so that the pups were prone to develop the disease when the appropriate trigger occurred. Activation of the virus, however, did not always occur during the life span of the parents, so that these animals could remain in good health. The inactivation process could be followed for several successive generations until the virus was activated in the progeny.53 It is now understood that some cancers of humans can also remain latent in the system until exposed to an activating agent. Even where a virus etiology has not been proven, as in human breast cancer, it is known that tumor cells can remain dormant for years or even decades. These cells may, however, lose their dormancy when new blood vessels arise in their vicinity and grow.54
Diet may influence the period of latency of cancer. The evidence for a link has been summarized in a well-known book, The China Study, written by Drs. T. Colin Campbell and Thomas M. Campbell II. The issue they were investigating was the ability of a classification of Group 1 carcinogens, the aflatoxins (generated by fungi growing on plant-food materials), to cause cancer. The initial inquiry, by L. D. Youngman and T. Colin Campbell, commenced in the Philippines, where they observed that the better-fed people experienced a greater incidence of liver cancer. The clue to this dilemma came when they discovered in their test animals that a high-risk factor was an abundant intake of protein (casein).55 In subsequent studies, this food item stimulated the growth of cancer cells, which would otherwise have lain dormant or progressed very slowly. Plant proteins tested (gluten, soy) did not have stimulatory effects even at high levels.56
Risk Factors for Some Cancers. The observation by the Campbells can be supplemented by additional information on risk factors for colorectal cancer. The World Health Organization recently has classified red meats as possibly carcinogenic (Group 2A) and processed meats as carcinogenic (Group 1).57 This represents the resurrection of an old idea mentioned by Moses regarding health outcomes as recorded in the Pentateuch (Lev. 3:17; 7:26; 19:26; see also Acts 15:29).
Meat eating is associated with an increased risk of colorectal cancer. Those who reduce meat intake generally increase the intake of plant-derived food components (with their protective chemicals), which accounts in part for protection. However, more specific information has come from a number of studies and most recently from human volunteers. Red meat has a rich supply of blood proteins and haem (myoglobin—muscles and hemoglobin—blood) associated with it. One suggestion is that these proteins react with other chemicals present in the digestive tract that are formed under the conditions normally present there and, further, that haem stimulates the formation of cancer-producing substances. As a result, carcinogens such as nitrosamines are made. Red meat is a much richer source of iron-containing proteins (particularly myoglobin) than white meat, thus potentially explaining its strong association with increased cancer risk. Processed meats also fit into the same risk category as red meats. It has been estimated by one group of researchers that the risk of contracting colorectal cancer is increased by 12 to 17 percent per 100 grams of all meat or red meat consumed per day; the risk is much higher for processed meats.58 While these estimates have been questioned, the World Cancer Research Fund recommends that those eating red meat should restrict intake to less than 500 grams per week. They noted that an individual eating a serving of red or processed meat daily for 40 years had a 20 percent increased risk of developing colon cancer. Individuals prone to eating meats cooked at high temperatures (grilling, frying, and barbecuing) increase their exposure to substances that are cancer producing, as do those who eat meats that are salted, smoked, and treated with nitrous compounds.59 The American College of Nutrition recently recommended that avoiding red meat has advantages beyond cancer-risk reduction and encompasses diabetes, hypertension, and cardiovascular disease. They went on to observe that all the nutrients contained in these products could be gained from plant-based diets.60
Nitroso-compounds interfere with cellular stability and cause stress. In practical terms, this means that these dangerous compounds are able to cause a lesion in the genetic material (DNA), injuring it and its ability to operate with fidelity. As a consequence, the cell’s physiological stability is lost, and cancer may develop. Such compounds are most abundant in dietary sources such as cured meats, seafood, and smoked cheeses.61
Those in ancient societies who took the advice of their prophets seriously and restricted the intake of blood through eating kosher or similarly killed meat (some still do this—Jewish, Islamic, and a few Christian groups) reaped health advantages, although they did not understand the reason (Lev. 7:26). The Bible is very clear about the inadvisability of eating foods containing blood. It is significant to note that this advice came again from the first church council held in the Christian era (Acts 15:20). The shedding of blood, whether of humans or animals, is a result of the entrance of sin into the world (Gen 3:21; 4:8–12). It should not stretch the imagination to think that the continual shedding of blood is not in God’s plan.
In the Jewish economy, God’s advice about the eating of blood was followed rather scrupulously, and today there is wide knowledge of kosher meats. The process of producing kosher meats involves draining the carcass of blood, removing prohibited fats and certain veins, arteries, and nerves. To remove the blood still in the meat, it is soaked in salted water.62 It is interesting to note that the carcass of animals such as sheep, pigs, and cattle, when slaughtered by traditional methods, actually contains around 50 percent of the original blood, with different muscles retaining more or less. Hence, the process of preparing kosher meat is rather detailed.
Prenatal Influences and Epigenetics
The idea that a pregnant woman’s diet has an effect on her child’s health has a biblical basis. Samson’s mother was instructed by God to use clean foods and drink non-alcoholic beverages during her pregnancy (Judges 13:3, 4, 7). Ellen G. White applied this advice to all mothers.63 Today, it is well-known that, at least for alcoholic beverages, the advice is accurate. This was not the only ancient association of fetal damage with drinking. The Greeks and Romans associated intoxication of the parents at conception to subsequent damage observed in the child. Much later observations (1700s) in Europe indicated that alcoholism in the mother adversely affected fetal development. However, clinical alcoholic syndrome was not recognized medically until 1968.64
Wider Applicability Suggested. Ellen G. White took the argument further and asserted: “Nor does it [transgression of nature’s laws] end with the transgressor; the effects of his indulgence are seen in his offspring, and thus the evil is passed down from generation to generation”65 (1890).
“Many suffer in consequence of the transgression [of the laws of health] of their parents. While they are not responsible for what their parents have done, it is nevertheless their duty to ascertain what are and what are not violations of the laws of health. They should avoid the wrong habits of their parents and, by correct living, place themselves in better conditions”66 (1905).
Foods Modify Us Genetically. Foods can modify the expression of genes and influences response to environmental risk factors. The chemical substances that surround heritable material (DNA) are able to modify the expression of genes in a cell. These substances are contributed to by the diet. And the modifications made may be inherited. The research on epigenetics suggests that obesity, diabetes, cancer, and some immune disorders are influenced by the prenatal diet. The heartening news is that some of these inherited tendencies can be modified by subsequent dietary choices.67 This means that what we eat and what our mothers ate influence our subsequent life history.
Foods of particular interest are folic acid, vitamin B12, and some bioactive substances from plants—garlic, broccoli, soybeans, and others. Making sure that there are adequate supplies of these chemicals can improve health outcomes because diet has an indirect effect on gene expression. The development of the early embryo can be adversely affected by high-fat diets and alcohol consumption. This field of endeavor is relatively new and is based on animal studies, so that knowledge applicable to humans is limited. However, it is beyond dispute that the bodily functions of animals and their response to risk factors or assaults by disease organisms are influenced by food intake. Poor choices early in the life of an individual appear to predispose to disease susceptibility later in life.68 This means that we and also our progeny are affected by our dietary choices.
Mycotoxins Present in Foods Eaten
Today, the scientific world and variable proportions of other groups are aware that molds are capable of producing toxins under certain environmental conditions. These are capable of causing illness and death.
Food Poisoning. The health reformers had some awareness of the dangers associated with eating decaying foods, for numerous cases of poisoning through consumption of moldy bread had been reported during the period 1826 to 1888, and deaths had been noted from eating moldy cornmeal from 1906 and 1909.69 The scientific evidence supporting such associations, however, was not particularly sound.
Against this background, the following statement was made in 1885 by Ellen G. White: “Cider and wine may be canned when fresh and kept sweet a long time, and if used in an unfermented state they will not dethrone reason. But those who manufacture apples into cider for the market are not careful as to the condition of the fruit used, and in many cases the juice of decayed apples is expressed. Those who would not think of using the poisonous rotten apples in any other way will drink the cider made from them and call it a luxury; but the microscope would reveal the fact that this pleasant beverage is often unfit for the human stomach, even when fresh from the press. If it is boiled, and care is taken to remove the impurities, it is less objectionable.”70
Two years later, she advised that fruit and vegetables showing any signs of decay should be avoided as follows: “Nicely prepared vegetables and fruits in their season will be beneficial, if they are of the best quality, not showing the slightest sign of decay, but are sound and unaffected by any disease or decay. More die by eating decayed fruit and decayed vegetables which ferment in the stomach and result in blood poisoning, than we have any idea of.”71
Food poisoning at this time was attributed to substances called ptomaines. Although this theory later proved incorrect, the principal components involved were known to be stable under boiling conditions. The presence of toxins in apples rotted by mold were not recognized until 1956 and the toxin was found in sweet cider some years later.72 During the 19th century, people did not commonly boil food to render it safe. In fact, a number of years after 1885, when pasteurization was introduced, a lively debate arose as to whether pasteurized milk led to human disease because it had been boiled. We now know that some mold-produced toxins remain very stable when heated.
Hence, it is difficult to sustain the claim that Ellen G. White’s statement came from scientifically based ideas of her day. Although it was known that apples were decayed by a specific fungus, the toxin produced (patulin) was not discovered until many years later (1943).73 In 1968, investigations revealed that heating canned apple juice at 80∞C. (176∞F.) for 10 minutes removed 40 to 50 percent of the toxin.74 This information coincides broadly with that indicated by Ellen White.
An entirely satisfactory explanation for the second statement is still being developed. However, it is known that common fungal disease organisms found on a range of plant products elaborate a number of toxins (i.e., Alternaria mycotoxins) in food items including citrus, tomatoes, nuts, oil seeds, and grains, with high levels of some toxins found in apples, tomatoes, and tomato paste. The toxicity of some of these fractions has been established in animals (toxicity to cells, interference with embryo development, tumor formation, hormone imbalance), but their overall effects on animal and human health are still being assessed. This appears to be the only group of toxins currently known that would fit Ellen G. White’s description of decay organisms producing toxins in a variety of fruit and vegetables.
The Modern Era Begins. Even though the patulin story was unfolding around 50 years ago, the dramatic significance of toxins produced by fungi was not recognized in the West until 1960 following the death of 100,000 turkey poults. A year later, it was discovered that rats fed peanut meal developed liver tumors and that the toxic substances involved (aflatoxins) were associated with fungi.75 It was evident that this was not a time for complacency, as peanuts were commonly used in certain parts of the world as an important human food item. Since that time various toxins generated by fungi have been found, particularly in cereal products. Some are highly carcinogenic and have been associated with liver cancer development in humans. Fungal toxins present in food items are of considerable significance to human health, particularly in the tropics where conditions favor growth of the organisms on grains, nuts, and even processed materials.
The toxin of particular interest raised in Ellen G. White’s first statement is patulin. This toxin can cause subacute effects in animals such as tremors, convulsions, ulceration, distension, and bleeding of the gastrointestinal tract. The toxin is harmful to the immune system at doses deemed equivalent to human exposure levels, and it may be deleterious to neurological health. Chromosome aberrations and mutations have been demonstrated in some animals, although there is no evidence of carcinogenicity. For these reasons, and owing to the fact that patulin levels remain high in apple products, there are concerns about the effect of fruit juice (particularly apple juice) intake on human health. These concerns have led to recommended limits in a number of countries.
The second statement highlighted above may refer to Alternaria toxins. These can interfere with reproduction and development in animals, some of which may develop tissue changes associated with cancer expression. In selected populations in China, where high levels of esophageal cancer are noted, there is a higher rate of contamination by various fungi capable of producing toxins. The initial suggestion made by Chinese researchers was that this might be attributable to Alternaria toxins. However, the more likely explanation is that complex interactions occurred among the toxins from Alternaria and/or from other fungi.76 This may mean that similar situations of multiple interactions in many parts of the world give an insight into Ellen White’s 1897 warning. At that time, ignorance about such toxins was almost absolute in the West. In Japan, a disease referred to as acute beriberi was first recognized in the last half of the 19th century. A variety of symptoms―from mild breathing difficulties and nausea to paralysis and death―were associated with the consumption of discolored rice. The first experimental determination of a link between illness in animals and consumption of damaged rice came in 1891. It took another 20 years for regulatory action to be taken by the Japanese government to protect human health.
Indeed, more study is required on the general question of the effects of disease in vegetables and fruit on human health, but the wise would avoid eating fruit, vegetables, nuts, grains, and derivative products containing diseased items, which is the main point of Ellen White’s advice. In practical terms, this also means avoiding discolored and broken nuts, which in peanuts carry a Group 1 carcinogen elaborated by a group of fungi.77
Health Principles Highlighted
Ellen G. White believed that the principles of health could be understood and that it was the duty of Christ’s followers to seek a thorough understanding of them. If advances in knowledge were followed, she held that practitioners could be respected leaders in their communities. Today we can rejoice in the clarity brought by science to many health issues. She advised us to listen to sources of instruction.78 Those who treat the human body as an edifice designed by God do well to respect this expert information and practice the principles of health daily.
The main ideas identified here as relating to risk minimization of acquiring non-communicable diseases are as follows:
● Moderation in eating is the key to achieving good health and longevity.
● Foods chosen for regular use influence the susceptibility of the body to non-transmissible diseases.
● Prenatal dietary choices influence the later health history of the child.
● Animal fats and red meats are prejudicial to health when ingested frequently and in large quantities.
● Vegetable oils are not all equal in their health benefits. Those containing saturated oils should be used sparingly.
● A vegetarian lifestyle, in which variety is the norm, is beneficial to health and promotes longevity.
● Highly refined foods and those with high sugar content predispose to obesity and various avoidable diseases.
● Food laced with fiery spices damage delicate tissues and predispose to disease.
● Salt-ladened food poses health risks.
● Colonization of food items by fungi, viruses, and bacteria frequently leads to the formation of mycotoxins, many of which have long-term and serious health effects.
Conclusion
Over the past 150 years there have been remarkable advances in the identification of causes of human diseases. Following the discovery of antibiotics and their widespread adoption since mid-last century and other advances in the field of microbiology, the incidence of contagious diseases has declined. Now the world is facing the danger of epidemics of non-communicable diseases that are related to lifestyle choices. Societies have invited and experienced these diseases for a long time, but they are now ravaging health. At the time when Ellen G. White wrote, she laid a firm foundation for maintenance of physical health by anchoring her advice to that of the Scriptures. She spoke about diet and the predisposition to disease when such ideas were not popular in society or medical circles. Her statements about cancer latency have been confirmed by modern science, and it is now known that diet can be a factor in cancer development. The sagacity of her early warnings against the use of foods invaded by microbes have been amply demonstrated by science, which has given some of the fungal toxins a Group 1 rating as far as carcinogenicity is concerned. Her general advice to avoid the excess use of sugar, fats, blood (in meat), fiery spices, and excess salt have been shown to be sound. The adoption of an lacto-ovo vegetarian diet (or similar) and eating in moderation, will protected those who follow her advice against the diseases of this age—cancer, heart disease, and diabetes. While she knew little in terms of medical science, her advice has remained relevant while that of many of her contemporaries has faded into oblivion and sometimes disgrace.
Christians might seriously consider her urging to understand and follow the principles of health. In today’s world, these can be derived from the biblical and scientific information available. Adhering to the best advice will give vibrant health, clear thinking, and an ability to understand the great truths revealed in Scripture. Following the principles of physical health prepares practitioners to recognize the great principles relating to social, mental, and spiritual health revealed in the Bible. This constitutes the urgent call given in Revelation 14—God wishes hearers to come out of the confusion and self-indulgence practiced in the present world. He wishes those who are honest seekers for truth to enjoy the benefit of these principles now and to prepare for the hereafter. The cry is, “‘Prepare to meet your God’” (Amos 4:12, NKJV).
Warren A. Shipton, Ph.D., is Professor of Microbiology, Asia-Pacific International University, Muak Lek, Thailand.
NOTES AND REFERENCES
